Cornea Consults and Surgery
By Board Certified Cornea Specialist, Carlindo Pereira, MD

The cornea is the clear surface of the eye. Since it is the first surface through which the light passes, a healthy cornea is essential for good vision. Cascadia Eye offers effective options for treatment of corneal disease, injury, and other conditions affecting the cornea. Our fellowship-trained corneal specialist, Dr. Carlindo Pereira, works with you to establish which procedure is best for your unique case. Corneal conditions can lead to visual deterioration and even complete vision loss, so it is necessary to have your eyes evaluated on a regular basis and seek treatment at the first signs of vision problems. With procedures such as corneal transplantation, pterygium surgery, and other options, we can reduce the symptoms and risks to your vision caused by corneal disease or trauma. Due to the specialized nature of cornea treatment, most appointments are made via a referral from your primary eye care provider.

Causes of corneal disease
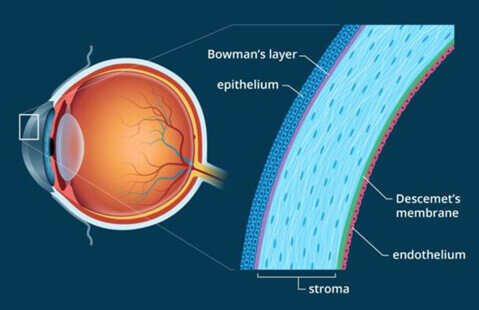
The cornea, a transparent covering of the front part of the eye, is made up of several layers: The epithelium, Bowman’s Membrane, the stroma, Dua’s Layer, Descemet’s Membrane, and the endothelium. Both the corneal clarity and the refractive power of the cornea play an important role in the cornea’s contribution to our overall sight. There are several conditions that affect cornea health.
Corneal disease can result from a variety of factors, including:
- Infection from wearing contact lenses
- Trauma or injury
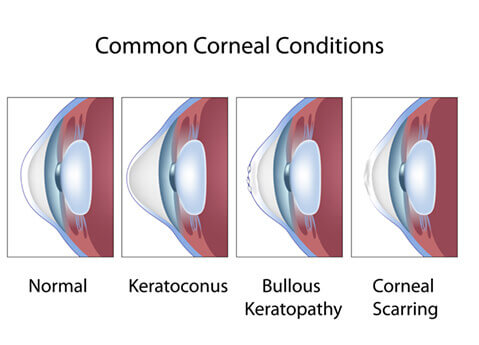
- Swelling or distortion of the cornea from eye diseases such as keratoconus, Fuchs’ dystrophy, or many others
- Corneal swelling after an eye surgery procedure
- Corneal scarring
- Corneal transplant procedures
- Penetrating Keratoplasty (PK)
Corneal conditions
Fuchs’ Endothelial Dystrophy
Fuchs’ Endothelial Dystrophy (Fuchs’) is a slowly progressive dystrophy of the cornea that generally does not affect vision until later in life. Signs of Fuchs’ can be observed for years without any symptoms or visual changes noticed by the patient. One of the first signs we notice are guttae, or small changes in one of the inner layers of the cornea. As this layer continues to change and thicken, it can lead to swelling of the cornea. If the most inner layer of the cornea, the endothelium, can no longer efficiently ‘pump’ the normal fluids from the swollen cornea, Fuchs’ patients may begin to notice a decrease in vision.
Generally a decrease in vision and any mild eye irritation is most noticeable to Fuchs’ patients in the morning, as the cornea does not pump out as much fluid while we are sleeping. Symptoms typically improve throughout the day. Once a stage of Fuchs’ is reached where it is affecting daily lifestyle activities, medical management is generally recommended. There are hyperosmotic drops to help ‘draw out’ the fluid, and in more severe cases, surgery may be recommended. Dr. Pereira, our corneal surgeon, is specialty trained in this area. There are procedures available, such as DSEK (Descemet’s Stripping Endothelial Keratoplasty) and DMEK (Deep Membrane Endothelial Keratoplasty) to transplant these most inner layers of the cornea if vision cannot be restored with just eye drops.
Keratoconus

Keratoconus is an asymmetric, non-inflammatory thinning of the corneas which causes an outward protrusion of the corneal tissue and thus an irregular surface of the cornea. While the exact cause of keratoconus is unknown, genetics is believed to play a factor. Keratoconus is generally managed with rigid gas permeable contact lenses to mask the corneal irregularity. Mild cases may be managed with glasses or soft lenses as the corneal irregularity may not drastically affect the vision.
Many cases of mild to moderate keratoconus are able to maintain 20/20 vision with the aid of rigid contact lenses. Surgical intervention can help to reduce some of the corneal irregularity in mild to moderate cases, but generally are not able to resolve all of the corneal irregularity. In severe cases, a corneal transplant (Penetrating Keratoplasty) may be necessary. Transplants are generally reserved for cases where visual acuity cannot be corrected to better than 20/50 (from corneal scarring), or when gas permeable contact lens wear cannot be tolerated.
Pterygium
Pterygium is a thickening of the outer eye tissue (conjunctiva) that gradually grows over the cornea, obstructing your vision. The cause is believed to be from the sun’s ultraviolet rays or exposure to a dry and dusty environment. People in tropical climates and those who are exposed to the sun for extended periods may be at higher risk for developing pterygium.
Symptoms of this abnormal growth of tissue include excessive tearing, eye discoloration, redness, irritation, increased astigmatism, reduced vision, and distorted vision. It may also cause scarring of the eye.
Symptoms caused by small pterygia can often be relieved with drops. This form of the condition usually only causes minor eye irritation. However, larger pterygia can impair vision and/or cause debilitating eye irritation, and may require surgery for removal. In addition to being a common problem, pterygium can also recur, even after being treated or removed. To reduce your risk of developing pterygium, you should take precautions to shield your eyes from the sun and environments prone to dust and wind.
Corneal ulcer and contact lens complications
A corneal ulcer is an inflammation, or possibly both an inflammation and infection of the cornea. A corneal edema is the swelling of the cornea caused by retention of tear fluid. Corneal ulcers or edemas can be caused by infections, contact lenses, chemical injury, trauma, and other eye conditions such as dry eye and severe blepharitis. Infectious corneal ulcers can arise from several types of bacteria, viruses, fungi, or even protozoa. These ulcers generally affect the most outer layers of the cornea, the epithelium and the anterior stroma, but severe corneal ulcers can penetrate all the way through to the most inner layers of the cornea and leave behind dense scarring.
Symptoms of corneal ulcers can range from a mild foreign body sensation and no vision loss, to severe pain and significant vision loss. Knowing the causative nature of the corneal ulcer can be extremely helpful in our treatment plan. Contact lens-related corneal ulcers are most often found in patients who over-wear their contact lenses and/or sleep in their contact lenses. Careful contact lens care and diligent lens replacement is considered preventative in many of these cases. Many contact lens complications such as “tight lens syndrome,” contact lens-related red eye, and a poor fitting contact lens may all mimic the beginning stages of a corneal ulcer, so it is always best to have the cornea evaluated if any eye pain or blurred vision occurs with contact lens wear.
Treatment for a corneal ulcer is dependent on the cause and severity of the infection and inflammation. General treatment begins with an antibiotic, but can vary significantly. Healing time for a corneal ulcer can take days for mild ulcers, and weeks to several months for more severe ulcers. If an ulcer has caused significant scarring to the corneal surface, a corneal transplant procedure may be recommended to help restore vision.
Other corneal dystrophies and degenerations
There are several types of corneal dystrophies and degenerations that can be inherited and in turn, may have a detrimental effect on vision and cause eye irritation. These dystrophies and degenerations may affect only one layer of the cornea or several layers of the cornea. One common dystrophy is Anterior Basement Membrane Dystrophy (ABMD). ABMD affects the most outer surface, or epithelial layer, of the cornea. Many degenerations and dystrophies, however, are quite rare. One example of a more rare degeneration is Salzmann’s Nodular Degeneration. Salzmann’s also affects the more outer layers of the cornea, including Bowman’s layer and the stroma.
Corneal transplant procedures
Descemet’s Striping Endothelial Keratoplasty (DSEK)
Less invasive than PK, and often with a shorter recovery time, is a procedure known as DSEK or DMEK. In the procedure, our eye surgeon will replace only the thin endothelial layer of the cornea with an organ donor’s cornea. There is less chance of tissue rejection with these procedures because most of the natural cornea is left intact. Plus, when compared with a full thickness corneal transplant procedure, DSEK and DMEK treatments often lead to quicker recovery time and a faster return of vision.
Penetrating Keratoplasty (PK)
If other, less invasive treatment options do not work, Penetrating Keratoplasty (PK), also known as Full Thickness Cornea Transplant, may be performed as a last resort. Dr. Pereira performs the surgery, which replaces the center of your natural, damaged cornea with a healthy tissue graft from a human donor. The procedure is designed to restore vision loss you had experienced as a result of disease or injury.
Other corneal surgeries
Superficial Keratectomy (SK)
SK is a procedure that is used to treat superficial ocular surface conditions, such as recurrent corneal erosions and anterior basement membrane dystrophy (ABMD). Many ocular surface conditions that cause damage to the most superficial layer of the cornea can be painful, and unfortunately, are often recurrent. The SK procedure is aimed at removing the area of damaged superficial tissue cells, which allows the cornea to regenerate its own healthier tissue cells. These cells take an average of one to two weeks to regenerate, and up to eight weeks to bond completely to the cells beneath it. SK is an outpatient procedure, and patients will leave the office with a bandage and a soft contact lens in place for comfort. Often, a regimen of topical antibiotic and anti-inflammatory eye drops will be used during the weeks following the procedure. Many patients with ocular surface conditions appreciate this procedure because it makes them less prone to recurrences of corneal damage, or reduces the number of recurrences in the future.
Contact Cascadia Eye
If you would like to learn more, or if you would like to schedule an appointment or consultation with our talented doctors at Cascadia Eye, please contact us today. You may also pre-shop for glasses at our online pre-shopping page any time. Our entire team is committed to protecting and improving your vision and the health of your eyes. We are happy to answer any questions you might have!
In addition, join us on Facebook, Instagram or YouTube to ask your questions about eyes, exams, and our practice. We’d love to hear from you – and there might be a blog to address your questions in the future.